|
Over the summer I had the chance to get to know more about Curio Wellness and more specifically the GI by Curio™ line. I had been using the products for a while to help my GI symptoms so getting to hear more about the creation and science behind the products was enlightening. The podcast episode I did with Chief Revenue Officer, Rebecca Raphael, covered some FAQs about medical cannabis usage along with some specifics about the formulation of the GI line. You can listen to that full episode here. I also shared a post highlighting some of my favorite GI by Curio remedies. Since the podcast and post went live I have received a ton of questions as well as requests for some more in depth details on the products I love and why they work. I’ve teamed up with Curio to address some of these topics and hopefully answer the questions you all may still have! The most popular question (and the one that I immediately had when I started considering the GI by Curio line) was what makes these medical cannabis products different? How are they different from just any cannabis product you’d pick up at your dispensary? A few things to call out here… First off, the CBG in the products is a game changer. In my recent podcast episode with Dr. Morris from Duber Medical she explained how CBG is a cannabinoid that has been found to target the gut. Having a formulation with CBG, CBD, and THC is a winning combination for addressing GI symptoms. The four products found in the GI by Curio line have varying ratios of CBG, CBD, and THC concentration depending on the ideal use. Each of the products has other unique differences which I will touch on later. Another big point of difference in the GI by Curio line is the involvement of Curio’s Scientific Advisory Board in product formulation. They ensure not only product safety, but also formulation to specifically address symptoms experienced by IBD, IBS, and other chronic gastrointestinal disease sufferers. Knowing that the products are created specifically for IBD patients gave me a lot of peace of mind when trying out the products for the first time. Another question I get asked frequently is about the THC potency and impairment due to THC. These products were created truly for medical use which means they kept the levels of THC as low as possible in order to provide maximum benefit with minimal impairment. Of course, I always recommend starting with a small dose since cannabis impacts everyone differently, but the goal of these products is to provide symptom relief not impairment. This is another factor that was really important to me when choosing medical cannabis products. A lot of the medications I was prescribed to treat my GI symptoms came with other side effects, one of which was extreme fatigue. I struggled to take these medications and then continue on my daily activities. So while my symptoms may be put at bay I was unable to function normally due to the fatigue. With the GI by Curio products I am able to control my symptoms and fully function since I do not experience impairment or other side effects while using the recommended dosing of the products. The last piece I want to touch on is when to use which products. Everyone has their own routine and product combinations that work best for them. I will share mine along with some of the key benefits/why I use these products in specific scenarios. Again, this is just my personal routine, what works for you may be different, but this could be a good place to start if you are just starting out with the line. The GI Comfort Tablets are my favorite for everyday use. They have a generous dose of both CBD and CBG which provide anti-inflammatory benefits as well and antimicrobial benefits. I take these as part of my daily routine and think of them sort of as a maintenance product. They aren’t necessarily for immediate pain relief or symptom relief, but over about a week of use I started to notice an overall difference in my daily symptoms. I also noticed this helped my anxiety levels even out when I first started taking the tablets regularly. The tablets are a great starting point if you are interested in dipping your toe in the medical cannabis world. They have an extremely low level of THC so you can expect no impairment when using this product. The next product that I love is the Soothe Tincture. I recently did an Instagram post about how much I love this product. I was able to replace my prescription anti-nausea medication with the tincture, which was a huge win for me. The Soothe Tincture was formulated specifically to target nausea. I had always heard that cannabis was a great remedy for nausea, but I was never confident enough in my knowledge to choose a strain or method that I thought would work without causing any impairment. This product was the answer. All the guesswork is taken out of the process and there are specific dosing instructions so you receive maximum benefit without the impairment. This has helped me with nausea related to my IBD as well as motion sickness. You consume the droplets under your tongue and symptom relief usually starts in about 20-30 minutes. Next up is the Soothe Vape. This is a great choice for immediate relief. If I am having active pain along with nausea this is my go to. It is formulated specifically to help with both nausea and pain while also providing a calming effect. This is helpful for managing nighttime pain and getting a better night's sleep. I also find this product very effective in soothing some of my joint pain that is associated with my Crohn’s Disease. Prior to switching to medical cannabis products like this one, I was prescribed different medications from muscle relaxers to opiates. These of course are not ideal for long term use and have many side effects (as well as potential addiction risks) that come with them. I am now able to find the same if not more effective relief without the risks and side effects. As someone who was always a tablet or edible girl, the vape seemed a bit intimidating, but dispensary staff can help make sure you are good to go and comfortable with your choice. Last up are the Stimulate Chews. Not to be dramatic, but these have been life changing. They have an even balance of CBG and THC. I usually take half of a chew which leaves me feeling better without any impairment. The effects are truly incredible though. These have helped me so much with pain relief, especially when I am experiencing cramping or stomach spasms. They usually kick in about an hour after I take one, sometimes quicker if I eat a small snack with it. These are a nighttime go to for me when I am in a lot of pain. They also help to ease my anxiety (often triggered by the pain and increase of symptoms) so it is a two in one fix. These were designed to help potentially increase appetite. I was worried (like I hear from many other patients) that it will swing the pendulum in the other direction and make you outrageously hungry. For me that has not been the case at all. Instead I describe the effect as making eating more bearable. If you are a GI symptom sufferer you know how excruciating it can be to eat when you are experiencing active symptoms. This has helped me be able to eat when before it was too painful. I also find if I eat something that starts to cause discomfort, taking a half of a chew can help make digestion of that feel less painful.
I can confidently say that in my experience all four of the GI by Curio products have contributed to symptom relief and improved quality of life for me. I am able to get relief from debilitating symptoms while still being able to participate actively in life and my children’s lives. I have shared my experience with many other IBD sufferers who have also seen benefits from these products and continue to use them in their daily lives. I hope this post helps to answer questions you may have. I am always open to sharing more about my experience and answering questions about my experience as well. To round out this post I just want to say a huge thank you to Curio for being so dedicated to providing reliable products that treat symptoms that IBD sufferers experience. It has been a relief to have a trusted place to turn to for medical cannabis products I can count on. With their commitment to safety and the involvement of their Scientific Advisory Board I feel confident that I am choosing a symptom management option that works and fits my lifestyle.
1 Comment
Recently I had the chance to chat with the creators of FODZYME and founders of Kiwi Biosciences, Anjie and David. I met Anjie earlier this year at Digestive Disease Week where I was introduced to the digestive enzyme powder. I immediately loved how the mission of FODZYME was to make foods more accessible to those with digestive struggles. So often the recommendation is to limit foods. This can feel extremely isolating and be difficult to stick to. FODZYME’s approach is to treat the food instead of eliminating it.
In this week’s episode of the Crohnically Mom podcast Anjie and David share the science behind the revolutionary powder. We discussed what FODMAPs are (these are what FODZYME targets), how the powder works, and who it works for. We also discussed the social and mental effects intense elimination diets can have on an individual and the benefit of having another option to try.
I have been using the powder when I eat certain foods since I discovered the product earlier this year. I know it personally works for me, but I loved being able to get an insight into why it works. I also really enjoyed hearing from Anjie and David about their journeys that led them to found their company and create FODZYME. Their passion for the product is inspiring and I am so grateful for their work.
You can listen to the full conversation in this week’s episode of Crohnically Mom. It is available on Spotify, Apple Podcasts, and Soundcloud. Additionally, if you are interested in trying FODZYME, they have provided Crohnically Blonde readers and Crohnically Mom listeners with a discount code (CROHNICALLYBLONDE) for 20% off your order! Antibiotic exposure is a risk factor that came up repeatedly during my time at Digestive Disease Week. I mentioned it in my recap of Pediatric IBD sessions, but there were many other sessions where it was a focus as well.
I surveyed my followers with IBD and about ⅓ of them said they think their onset of early IBD symptoms correlated with a time of heavy antibiotic usage. Of course, this isn’t a scientific study, but I thought it was interesting that this is a factor the IBD community can identify firsthand. The CDC has identified the overprescribing and improper use of antibiotics to be an issue in the United States. In a 2022 study, the CDC reported that at least 28% of all antibiotics prescribed in an outpatient setting were unnecessary. That is 28% of people unnecessarily exposed to a key IBD risk factor. A lot of our country’s reliance on antibiotics as a first line of treatment can be linked back to the flaws within our healthcare system. Instead of focusing on an underlying issue, our culture is prone to immediately jumping on a “quick fix.” Providers are incentivized to see as many patients as possible. It is easier and quicker to write a prescription and send a patient on their way as opposed to taking a holistic look at the patient’s health to identify other potential causes for their symptoms. This isn’t to fault providers. There are many of them who wish to take a more holistic approach, but the way our healthcare system works doesn’t allow them to. Patients are not blameless in this either. As patients we are conditioned to have a medicine to fix just about everything. If we go to a doctor for a cold and they tell us to go home and get some rest, we leave grumbling about how we made the trip and made a copay just to be told to go home and get some rest. It is almost like we want them to unnecessarily tell us we have a sinus infection so we can get some antibiotics and feel like we are doing something to heal quicker. I have actually heard people leave urgent care complaining that they couldn’t get an antibiotic prescription and planning to just “go see another doctor until they get one.” Moving away from antibiotic overuse is a cultural shift. It can’t just be on the provider or patient side, it has to be a collaborative effort. There also needs to be more openness in the discussion of natural (or non prescription remedies). So often if you mention a natural or holistic treatment, a provider will dismiss the suggestion. Of course sometimes these treatments are totally bogus and not worth your time, but in other scenarios they could have potential benefits with few to no downsides. For many of these holistic treatments, we are still lacking evidence based research that support them. It is responsible of a provider not to suggest something without supporting evidence, but it is also irresponsible for them to shut down the conversation altogether. With the CDC pushing us toward less antibiotic use, will there in turn be more money and research dedicated to other holistic treatments? The last factor I want to touch on is insurance coverage for medications. So often, antibiotics are not only a seemingly “quick fix,” but also a cheap one. Insurance companies are more likely to cover antibiotics than they are any type of alternative treatment. Even if a doctor recommends something like acupuncture to help with sinus pain, it is not likely to be covered under many insurance plans. Do you know what is covered? That 7 day supply of an antibiotic to treat a “potential sinus infection.” Again, I want to reiterate that this is not the fault of providers or the fault of patients. We as a society have gotten to this point and need to recalibrate on what is best for our country’s health as a whole. I am also a firm believer that antibiotics are 100% necessary in some situations. I will give my kids antibiotics if they need them. I take antibiotics when I need them. Antibiotics can save lives when used appropriately. Just like so many things in American culture, we have taken them to one extreme. If we can find a way to balance antibiotic use, I predict our society will see positive health benefits. To get there though, we have some big changes that need to be made. xx
Recently I had the chance to sit down with Tamara Duker Freuman, registered dietician and GI nutrition expert. I interviewed her for my podcast, Crohnically Mom, and she provided helpful insight into navigating nutrition and IBD. You can listen to the interview here.
How I was introduced to Tamara was through her newest book “REGULAR”. It is one of the most helpful books about GI symptoms I have ever encountered. Many books focused on addressing GI symptoms focus on things you are doing wrong – the wrong diet, not getting enough sleep, eating “bad” foods, etc. This is demeaning for a reader, especially one with IBD. A lot of the time we have tried everything and it hasn’t worked so the generalized assumption that people with GI issues can “do something about it” is incredibly frustrating. “REGULAR” has a totally different tone that I would describe as empowering.
Tamara starts the book by providing a thorough, yet completely understandable, explanation of how your digestive system works. This is one of my favorite parts of the book and we were only in the first few pages. She breaks down the anatomy in a way that doctors rarely do during a 15 minute appointment or if they do, it usually isn’t communicated in a way that is, excuse my pun, digestible. This knowledge is so crucial because it allows someone experiencing GI symptoms to accurately explain to their doctor what they are experiencing. It also saves them from hours of Google research and perusing through unverified information. This is straight to the point, reliable information about what the heck is going on in your digestive tract. After the helpful introduction, Tamara guides you through a quiz. The quiz allows you to answer questions about your symptoms and narrow down the chapters that could be most relevant to you. Most people are reading this book not for their interest in GI disorders, like me. They are looking for help, a solution. This quiz helps them get to the most relevant information quickly and because of that, I love this style of book for non-fiction reads. The chapters address a range of GI symptoms/issues from Irritable Bowel Syndrome, to pelvic floor dysfunction, to Inflammatory Bowel Disease. The IBD section was where I spent most of my time. I was looking forward to hearing Tamara’s recommendations, but I admit at first I was a bit nervous. Usually I get nervous reading any book that mentions “diet”. So often they are filled with unrealistic overhauls of your current lifestyle that put foods into categories of “good” and “bad”. As someone who has struggled with an eating disorder in the past, this can be very triggering and also just not helpful. “REGULAR” is refreshing as it doesn’t do either of these things. Tamara explains how foods navigate through your system and how they are absorbed. She never says “do not eat this.” Instead she suggests ways to make certain foods more tolerable (e.g. changing their consistency). You will hear in our conversation, how passionate in her practice Tamara is about providing customized nutrition counseling. She isn’t about just throwing a blanket “fix all” meal plan out there and hoping it works, so she doesn’t do that in “REGULAR” either. Overall, this book is full of fresh takeaways even for someone who is not new to being a GI patient. Tamara’s approach is meant to leave the reader feeling empowered, whether it’s speaking to their provider, looking for answers to their symptoms, or exploring a type of food they always thought was out of reach. This will now be a “go to” recommendation from me for anyone suffering from a GI condition. You can hear my in depth conversation with Tamara on this week’s episode of Crohnically Mom. You can also grab Tamara’s book, “REGULAR”, on Amazon. xx Traveling is one of my greatest joys in life so when I was diagnosed with Crohn’s Disease, I refused to let my symptoms prevent me from doing what I love. Flying can be a big source of anxiety for those with Inflammatory Bowel Disease. There are many factors that can play into the feeling, but one of the most common ones is the concern about not being near a bathroom. Flying is also a necessity in some situations - work travel, family visits, etc. Your travel schedule and GI symptoms unfortunately don’t coordinate to make sure you have a comfortable experience. That being said, anything to reduce the anxiety around flying when experiencing GI symptoms is a welcome suggestion. One of the most simple ways to combat a common concern is to make sure you are positioned near a bathroom on the flight. On certain airlines, you can choose your seat ahead of time. This means locking in that prime aisle seat right next to the facilities. No stepping over other passengers mid bathroom emergency and you are close by so you won’t have to fumble down the aisle as you’re trying to make it to the facilities. This is great for airlines that offer this preselection option.This isn’t always the case, though. I most frequently fly Southwest which has open seating (i.e. no preselected seats). This has caused me a lot of anxiety over the years - panicking when I didn’t get an early boarding group, having to ask passengers to switch seats with me and awkwardly explaining why, and trying to do anything I could to avoid having to use the bathroom on flights (which was not very effective). A few years ago, I saw some fellow IBD patients share a travel tip and it instantly changed traveling for me. Southwest offers disability preboarding and Inflammatory Bowel Disease is a disability. When I first found this out, I was in the stage of denying IBD was a disability that impacted functions of my life, but now looking back I wish I would have accepted this sooner so that I could utilize the resources that are there for IBD patients. That is why they are there, to help us! I check in like I normally would for my Southwest flight and once I get to the gate, I speak with the gate attendant. I explain that I require disability boarding due to my Crohn’s Disease and need to be seated next to a bathroom. I always have my doctor’s note on hand to show if it is needed. The gate attendant updates my boarding pass to list preboarding status and I am good to go.
Disability preboarding includes passengers with all types of disabilities. This means you will often be boarding with wheelchair users and other passengers with mobility challenges. I understand that for them it is more necessary that they have the seats closer to the front of the plane, while for me I have the option of sitting near the rear bathrooms. That being said, I make sure not to take the front seats if they are needed by others. When I board the plane, I confirm with a flight attendant that there are functioning bathrooms at the back of the plane and head on back to secure my seat. This small tweak to my travel routine has made a significant impact on my anxiety level while traveling. The knowledge that I will be able to have easy access to a bathroom while in the air is a huge comfort. I recently realized how many fellow IBD patients don’t know that this is an option. I didn’t for the longest time, until I saw a patient advocate share the information ( I wish I remembered specifically who because I would definitely shout them out!). I know how much that information helped me so I want to help spread the word that Southwest does offer this option to support passengers with visible AND invisible disabilities. As I mentioned before, I went through a period where I was in denial that IBD was a disability. For a while when I started to actually utilize these types of programs, I would feel embarrassed. I thought people were looking at me strangely because they couldn’t see that I was sick. I went out of my way to awkwardly over justify why I needed certain accommodations. It has taken me years to work through and I still struggle with it, but I have gotten a lot more comfortable. Just because my condition isn’t visible doesn’t make me any less deserving of the programs that are in place to assist people like me. I am not saying to utilize every offered accommodation “just because,” but if it is something that will impact your condition, symptoms, or quality of life, you should feel empowered to use these resources that are there for you. As an IBD patient did you know that this was an option for you? How would an accommodation like this impact your travel experience with IBD? xx
At the beginning of my IBD journey, I had the pleasure of working with Oshi Health in their early days. At the time, they were mainly a tracking app for GI symptoms. My mom and I attended a user research group in New York and met with some of the consulting physicians. This was the first time I was introduced to the concept of integrative care. It wasn’t something that was a reality yet for many patients, but the idea that providers could work together and treat the whole person was a positive one.
Almost 5 years later, I had the pleasure of sitting down with Michael Currier, a GI Physician Associate at Oshi Health, to get an update on how the company and the app have evolved. Oshi Health has grown from a tracking app for GI conditions to a full service option for receiving integrative GI care. Through the app, you are matched with an Oshi GI provider who you see virtually. The appointments are on average around 45-minutes as opposed to the usual in office 10-15 minutes that are standard practice for most of us. Your provider gets to really know you and dig into the whole story your body and symptoms are telling. They can order labs or diagnostic procedures for you with their local partners (they have a scheduling team that takes care of this for you!), and you are matched with an entire team of providers at Oshi. They understand that the best GI care is multifaceted and consideration needs to be given to the effects both diet and mental health have on GI conditions. Through Oshi, you are paired with a Registered Dietician and a GI Psychologist to help you feel better from all angles. The best part, in my opinion, is that your GI provider, dietician, and psychologist all work together behind the scenes to collaborate on the best care plan for you.
A few other highlights for me are: they will work with a doctor you are already seeing if you want additional support, but aren’t ready to make a complete switch and you have access to your Oshi team via chat so you never are without a line of support. Another important call out is that they partner with many insurance companies that will cover your care through Oshi.
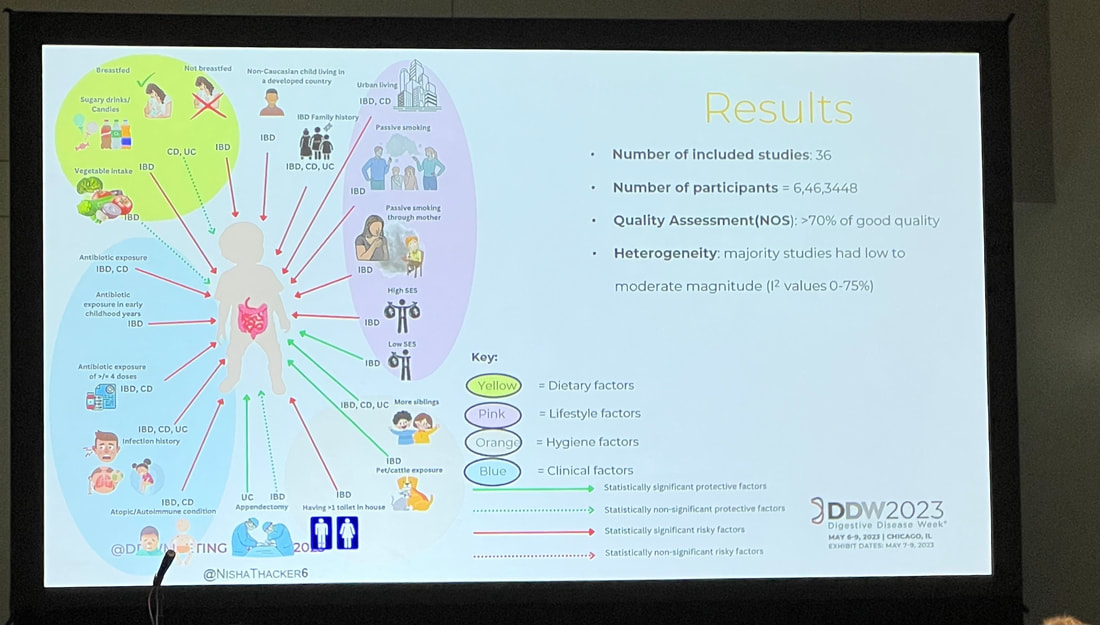
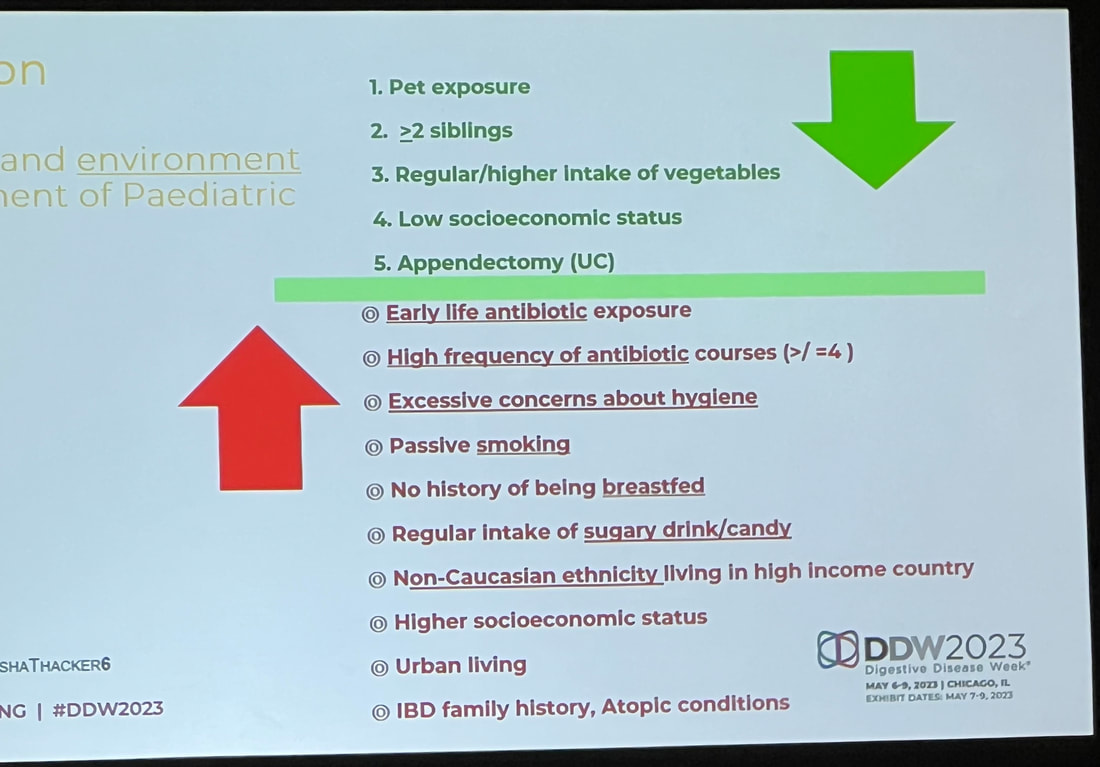
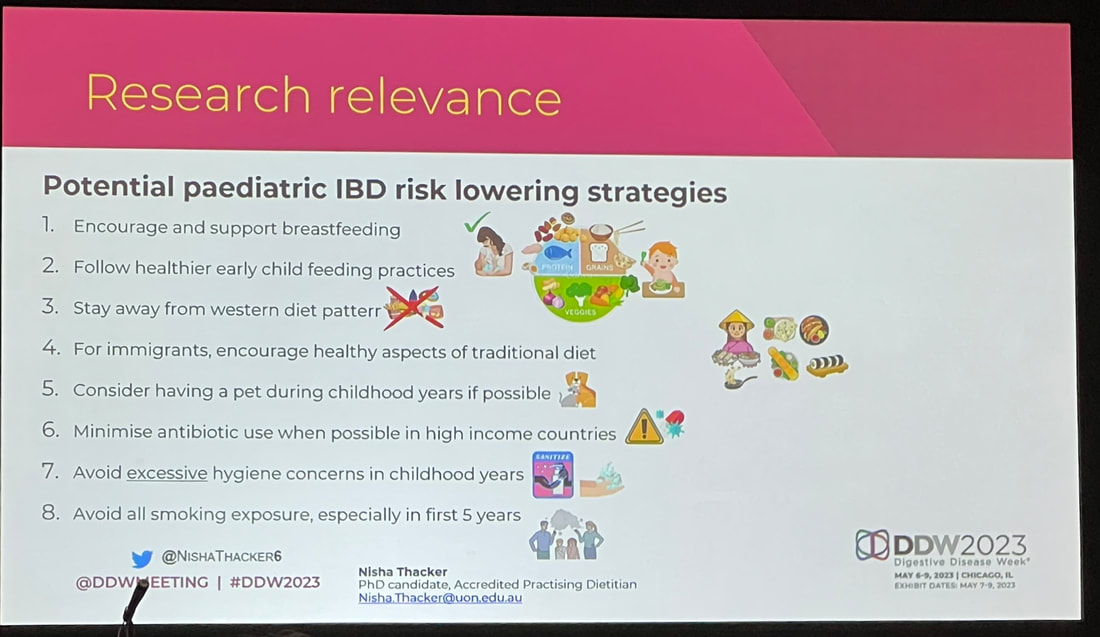
On an individual level, Oshi Health is changing the game for patients. They are breaking down barriers of accessibility when it comes to GI care. They are empowering patients by treating them as a whole person, not just patients. This is also revolutionary for our healthcare system in general. It is rare that there is so much collaboration between different providers despite how much of a positive impact it could make. Oshi Health has designed a model that flips that statement on its head and is challenging what we currently accept as the status quo. You can listen to my conversation with Michael Currier from Oshi Health on this week’s episode of Crohnically Mom. He explains more about the benefits of integrative care, how Oshi is creating more accessible GI care, and how their model gets patients better. One of my favorite sessions at DDW focused on pediatric IBD. This is a topic that is near and dear to my heart as members of my family have been diagnosed with IBD in childhood and I know my own children are at a greater risk. Nisha Thacker, an Accredited Practicing Dietician at Sydney Children’s Hospitals Network in Australia, presented her team’s findings, which provided some very valuable insight into pediatric IBD risk factors, but also left me with some questions. I am going to share some slides with key takeaways I gained from the presentation and share my thoughts on the findings from the perspective of a patient and a mom. A few background pieces of information that were shared prior to reviewing the findings were:
Nisha shared a diagram mapping out the influence of dietary, lifestyle, hygiene, and clinical factors and their effect on pediatric IBD risk, which I share below. Many of the factors that have a negative impact on IBD risk are commonplace in our Western society. Western diet in general is a risk factor, but there are a lot of factors that paint the picture of middle class or upper class Western life. Things like having more than one toilet in a home, urban living, and early antibiotic exposure are all contributing risk factors. On the other hand, having more siblings, being exposed to pets or cattle, and not being formula fed are all contributing factors to lower IBD risk. I thought the most telling though, was that a non-Caucasian child living in a developed country has a higher risk of developing IBD. You can’t review this information without thinking to yourself that maybe we are doing something wrong here in the West. In other cultures, there is a greater focus on holistic treatments instead of jumping straight to antibiotics. There are larger, generational households with more children. Mothers have more family and societal support postpartum, which encourages successful breastfeeding. There is less consumption of sugary or processed foods, and really a different dietary structure. Our lifestyle in the West does not bode well for avoiding the development of IBD. One of the things that really struck me about these findings was the impact that not breastfeeding has as a risk factor for IBD. I found this interesting because this is identified as a negative factor in other pediatric and maternal health outcomes. If we know that supporting a mother to breastfeed will influence pediatric outcomes then why don’t we have more support? Why do we not have adequate maternity leave to support breastfeeding mothers? Why do we not have healthcare coverage that universally provides continued lactation support? I would love to see a study on IBD rates in countries with longer maternity leave or countries with higher breastfeeding rates. This also speaks to parental support as a whole. Western culture does not champion multigenerational households like other countries and cultures do. With multigenerational households come additional people to help – whether that be in watching older children so a mother can breastfeed, preparing homemade meals for the family, or having more adults contributing to a family’s income so maybe a mother can stay home with her newborn longer. This isn’t always the case, but I think it could be worth diving into. The biggest takeaways I have as a parent are what I can do to lower the risk of IBD for my children. There are things I can’t change, like genetics or the fact that my children had to be at least partially formula fed, but there are things I can do that can make a difference.
Pet exposure is a big one that is actionable. I am working to get more information on the science behind this, but unrelated to IBD our pediatrician has mentioned the benefit of having a dog in building stronger immunity as a child. I am putting a pin in this and I hope to come back with more information. The other two easily actionable factors are diet (higher consumption of vegetables, lower consumption of sugar/candy) and antibiotic exposure. To be clear here, I believe that antibiotics are necessary in some cases and can save lives. The recommendation isn’t to never expose your child to antibiotics, it is to expose them only necessarily. The same goes for diet. This study won’t motivate me to never let my kids have cupcakes again, but it will encourage me to continue packing their diets with vegetables any chance I get. I do want to address the factors that we can’t control or we choose not to. “Mom guilt” rang in the back of my mind during this whole presentation. When I originally posted these slides on my Instagram, I received countless messages of moms freaking out. It is our nature to want to do whatever we can to protect our children, but some things truly are out of our control. I wanted to call out a few things in particular. Low socioeconomic status is an identified “protective factor” in avoiding IBD, but has many other potentially negative effects on a family. This study is viewing that data in a bubble as opposed to the whole impact of low socioeconomic status. Having more than two siblings is another “protecting factor” in IBD development. This again is something that is being looked at in a bubble. There is no recommendation to have more children for the sole purpose of protecting against IBD. The same goes for other factors such as urban living. There are some benefits in other regards when it comes to urban living. We can’t just change where we live to hopefully avoid IBD. As a mom to two little ones, there are two factors that give me a pit in my stomach. One is the risk factor of not being breastfed and the other is early life antibiotic exposure. Breastfeeding is something that is so deeply personal and challenging. Sometimes there are medical reasons (physical or mental) that prevent breastfeeding. Other times mothers are not able to breastfeed due to lack of resources or support. There are also scenarios where breastfeeding is not an option at all. This is such a complex issue and emotionally charged on both sides. As a mom, if you read this and get a pit in your stomach, try to remember that this information is again, in a bubble. Just because you didn’t breastfeed does not mean your child will have IBD. The same goes for early antibiotic usage. This is something that can be out of a parent’s control. If a baby has an infection that needs to be treated with antibiotics, that is the best course of action. There are situations where the benefit outweighs the risk and there is nothing that can change that. In conclusion, this session provided some very interesting insight and shared some low risk lifestyle changes that we can adapt to help lower our children’s risk of IBD. On the other hand, I am curious to see additional studies that evaluate these factors on the basis of risk/benefit. I also am interested to see how the findings may change if the study was conducted outside of a Western environment. What questions do you have after reviewing and reading? Are there any key points you would want to hear more about? Here are my top share worthy pieces of content I've stumbled across in the past week! This list is a little shorter than usual because (if you've been following along you know) I unplugged for a bit to do Disney World with my family. Now that I am getting myself back up to speed, here is what has caught my eye.
April was Alcohol Awareness Month - @neda did a great post sharing that about 20% of eating disorder patients develop an alcohol use disorder. This week at Digestive Disease Week I have also been learning about the correlation between IBD and developing an alcohol use disorder. This topic is very top of mind for me right now and I like that this post highlights some resources for those looking for support. May 4th was the first Terminated for Medical Reasons Awareness day. This topic is an emotional one and often hard to talk about, but with abortion rights continuing to diminish we need to be talking about this. @postpartumsupportinternational shared a powerful post about one mother's experience with TFMR and her explanation of why it is so critical to protect this right. NPR on Messy House Shame - My mom actually sent me this article because she knows how hard I stress over keeping my home together. This article provides some relief in validating that you are running your home just the way you are supposed to for your family. I'm kicking off your week with a roundup of content I've found really valuable over the past two weeks! The last roundup was a hit so I am even more excited to share a bit of what has been filling my content plate recently. Always feel free to drop a link to your favorite article, podcast, or post you "saved" this week. I would love to check it out! This week...Black Maternal Health Week - Posts & Resources
Black Maternal Health Week was 4/11-4/17 so I wanted to first and foremost highlight some of the resources related to the topic. The Womb Room, a Baltimore based perinatal support center, shared a post on Instagram that pointed out so harrowing statistics about maternal mortality rates for black mothers. This post serves as a somber reminder of the disparity in healthcare and the importance of bringing awareness to this issue. The post doesn't just share WHY we need to care, it also shares specific ways that you can make an impact. We shouldn't just wait for this week to occur to bring awareness to this issue. This needs to be at the forefront of our minds constantly until changes are made. This article on The Every Mom from a couple years ago is also very helpful if you are looking for a deeper dive into the disparities in Black Maternal Health and some suggested ways to help. Addressing Healthcare Inequity with IBD Advocate @kimberlymhooks Kim and I are both part of the American Gastro Association Patient Influencer Program. That is how I discovered her content and have been finding everything she puts out to be so helpful. She is a great follow for those in the IBD community. She shares a lot about her life with IBD and the advocacy work she is doing all with an incredibly positive attitude. 78% of the Mental Load Falls on Mothers with @mamapsychologists Mental load is a hot topic right now and rightfully so. We are finally putting a name to all of the extra work that moms do and recognizing that work. It's not just magic behind the scenes, there are hard working mom's making life happen. This post really spoke to me as I recently recorded a podcast episode about the mental load of traveling as a mom. Podcast: Skimm This: State of Women... and Society My last pick of this week is a podcast. The Skimm just launched Skimm This Special Edition where they are diving into different issues impacting women in America. The first episode called State of Women... and Society was one of the best podcast episodes I have ever listened to. It so eloquently described the social landscape we are facing as women and even had the author of Fair Play on to weigh in. The Fair Play card game has been a game changer in my marriage after having kids so I was thrilled to hear more about how this tool can help other women. The second episode of the mini series dropped a few days ago and it is at the top of my queue to listen to while working this morning. As someone with IBD, aches and pains are just part of the package, but IBD may not be the only culprit. Since my diagnosis in 2015, I have heard providers mention in passing the link between Crohn’s Disease and other autoimmune conditions. Sometimes this correlation was used as a potential cause to pin unexplained symptoms on, but I never really got to the point of a secondary diagnosis. For years I have been complaining of aching and swollen joints even after my Crohn’s symptoms improved and I was steadily receiving treatment. Eventually, my providers suspected that this chronic pain could be caused by something other than just IBD. After years, yes years, of being urged to visit an arthritis specialist, I finally did.
So what made me decide to go? The statistic that up to 30% of IBD patients also suffer from arthritis or joint inflammation has been living rent free in my head for years. But to be fair, I’ve had a lot going on over the past few years. With the pandemic, the birth of my kids, job changes, moving, etc. it has been a whirlwind. I already spend so much of my time at doctor’s appointments so the thought of having to add yet another specialist into my rotation was not appealing. I wasn’t motivated to go get my joints checked out. Yes, it was affecting my daily activities, but it didn’t seem like an urgent situation. Plus I was having so much pain following each c-section, how active could I really be even if my joint symptoms somehow magically improved? Following the birth of my daughter and the numerous complications I experienced, I began intensive physical therapy to rehabilitate my abdominal muscles. I have been blown away at the improvement I’ve seen, and surprise, I’ve actually been able to be more active. Walks around the neighborhood, carrying my kids through the mall, and running on the playground have all become activities that I am able to do, and want to do. Unfortunately, my joint pain was still persistent despite the improvements through physical therapy. The more I realized what activities I could be doing, the more frustrated I got at the discomfort I experienced. The biggest factor that encouraged me to finally see a doctor was my kids. Of course the pain and frustration had been present before. In fact, I remember leaving yoga class at the YMCA crying because at 25 my joints were more swollen than the geriatric participants that made up the rest of the class. With my kids though I want them to experience me as the best mom possible. For me, part of that was taking steps to get to the bottom of my joint pain. This morning I had my first appointment with a provider that specializes in arthritis care. I’m in the process of completing various bloodwork and scans to help figure out the actual cause of my joint pain, so it may be a while before I know a definitive answer or see improvement. I do feel confident, though, that I have made steps in the right direction. I am hopeful that this road to a diagnosis won’t be as turbulent as it was with my Crohn’s diagnosis. I have some experience under my belt now and am more confident navigating medical appointments. What makes me feel most positive though are the stories and advice I’ve gotten from the online IBD community. At least if I have to go on this journey, I have some very inspiring peers helping me and cheering me on. |
Blonde babe.
Millennial mom. Crohn's crusher. Mental health advocate. Sharing my raw and real journey through motherhood and navigating Crohn’s Disease. CrohnicallyBlonde is a place where I serve up my unfiltered commentary on chronic illness, mental health, pregnancy, and motherhood alongside lighter lifestyle content like beauty product reviews, travel tips, and book recommendations. My hope is that by authentically sharing my story I can help others going through similar situations not feel so alone and maybe even laugh along with me. categories
All
archives
November 2023
|
|
LET'S CONNECT ON SOCIAL
|
ContactFor press, partnerships, and general inquiries please contact: [email protected]
|















 RSS Feed
RSS Feed