|
One of my favorite sessions at DDW focused on pediatric IBD. This is a topic that is near and dear to my heart as members of my family have been diagnosed with IBD in childhood and I know my own children are at a greater risk. Nisha Thacker, an Accredited Practicing Dietician at Sydney Children’s Hospitals Network in Australia, presented her team’s findings, which provided some very valuable insight into pediatric IBD risk factors, but also left me with some questions. I am going to share some slides with key takeaways I gained from the presentation and share my thoughts on the findings from the perspective of a patient and a mom. A few background pieces of information that were shared prior to reviewing the findings were:
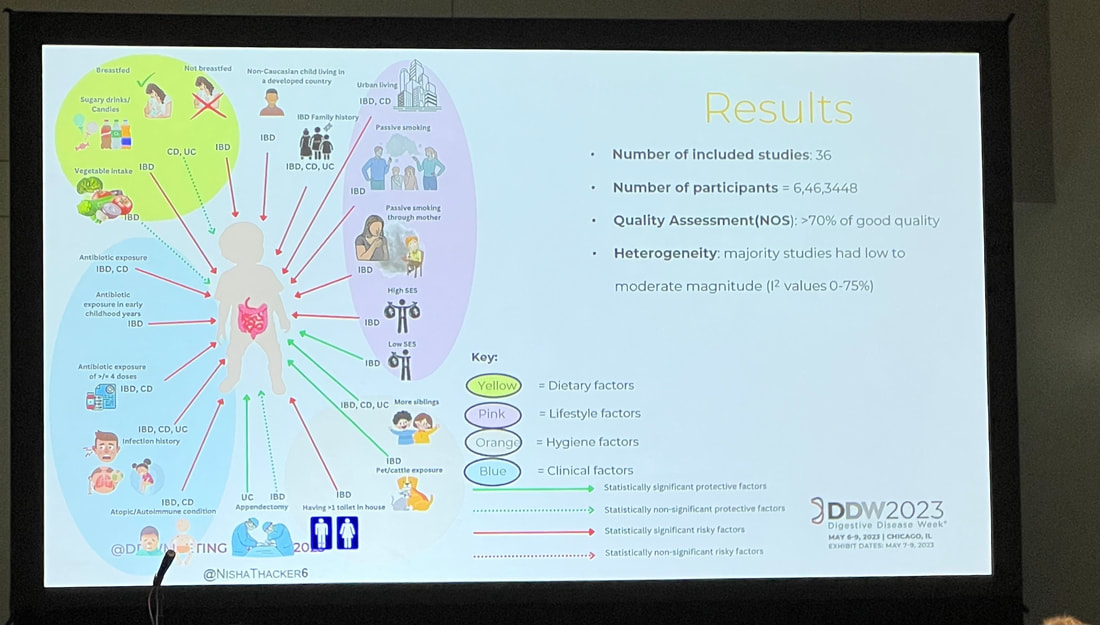
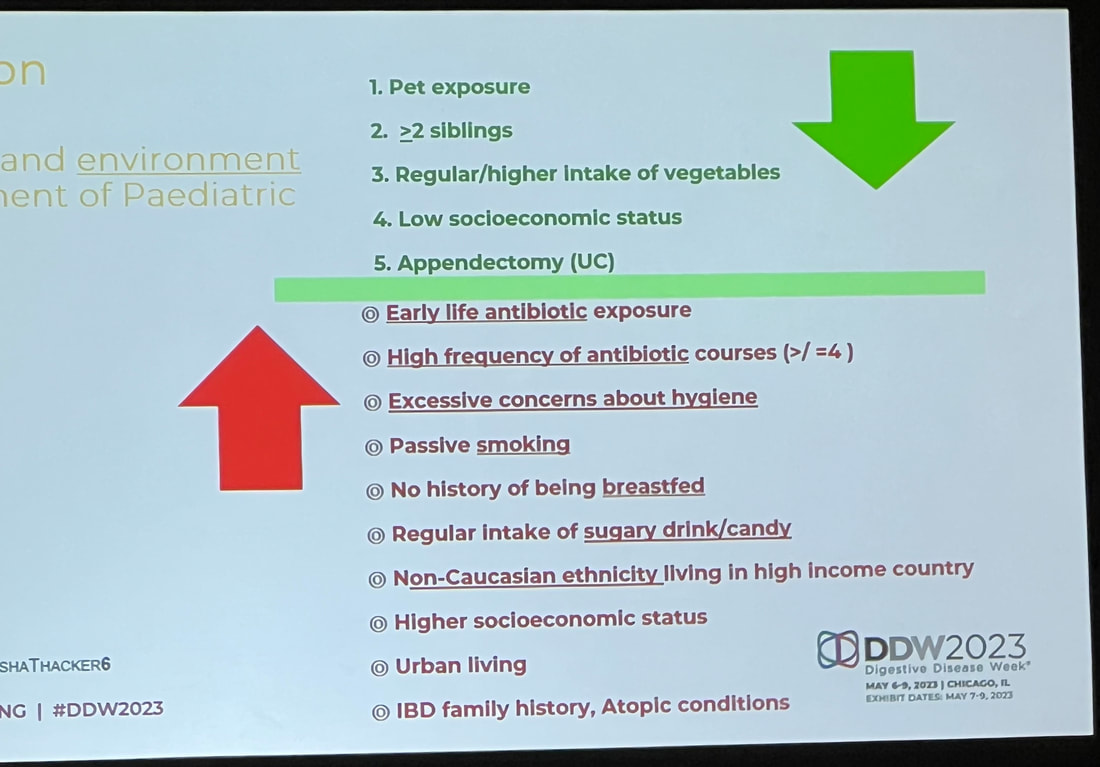
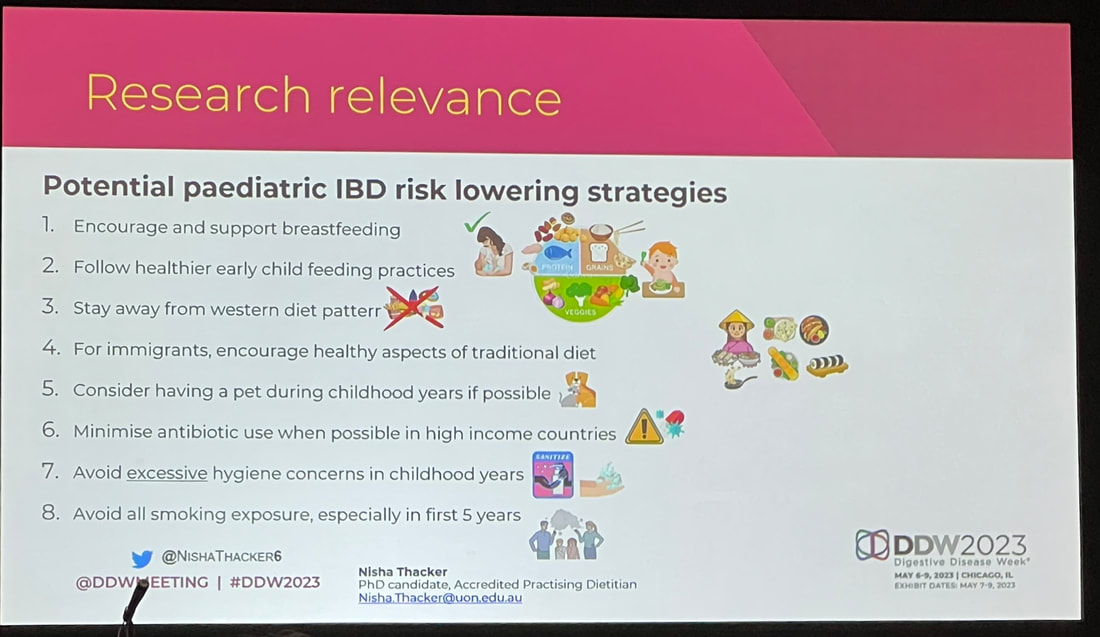
Nisha shared a diagram mapping out the influence of dietary, lifestyle, hygiene, and clinical factors and their effect on pediatric IBD risk, which I share below. Many of the factors that have a negative impact on IBD risk are commonplace in our Western society. Western diet in general is a risk factor, but there are a lot of factors that paint the picture of middle class or upper class Western life. Things like having more than one toilet in a home, urban living, and early antibiotic exposure are all contributing risk factors. On the other hand, having more siblings, being exposed to pets or cattle, and not being formula fed are all contributing factors to lower IBD risk. I thought the most telling though, was that a non-Caucasian child living in a developed country has a higher risk of developing IBD. You can’t review this information without thinking to yourself that maybe we are doing something wrong here in the West. In other cultures, there is a greater focus on holistic treatments instead of jumping straight to antibiotics. There are larger, generational households with more children. Mothers have more family and societal support postpartum, which encourages successful breastfeeding. There is less consumption of sugary or processed foods, and really a different dietary structure. Our lifestyle in the West does not bode well for avoiding the development of IBD. One of the things that really struck me about these findings was the impact that not breastfeeding has as a risk factor for IBD. I found this interesting because this is identified as a negative factor in other pediatric and maternal health outcomes. If we know that supporting a mother to breastfeed will influence pediatric outcomes then why don’t we have more support? Why do we not have adequate maternity leave to support breastfeeding mothers? Why do we not have healthcare coverage that universally provides continued lactation support? I would love to see a study on IBD rates in countries with longer maternity leave or countries with higher breastfeeding rates. This also speaks to parental support as a whole. Western culture does not champion multigenerational households like other countries and cultures do. With multigenerational households come additional people to help – whether that be in watching older children so a mother can breastfeed, preparing homemade meals for the family, or having more adults contributing to a family’s income so maybe a mother can stay home with her newborn longer. This isn’t always the case, but I think it could be worth diving into. The biggest takeaways I have as a parent are what I can do to lower the risk of IBD for my children. There are things I can’t change, like genetics or the fact that my children had to be at least partially formula fed, but there are things I can do that can make a difference.
Pet exposure is a big one that is actionable. I am working to get more information on the science behind this, but unrelated to IBD our pediatrician has mentioned the benefit of having a dog in building stronger immunity as a child. I am putting a pin in this and I hope to come back with more information. The other two easily actionable factors are diet (higher consumption of vegetables, lower consumption of sugar/candy) and antibiotic exposure. To be clear here, I believe that antibiotics are necessary in some cases and can save lives. The recommendation isn’t to never expose your child to antibiotics, it is to expose them only necessarily. The same goes for diet. This study won’t motivate me to never let my kids have cupcakes again, but it will encourage me to continue packing their diets with vegetables any chance I get. I do want to address the factors that we can’t control or we choose not to. “Mom guilt” rang in the back of my mind during this whole presentation. When I originally posted these slides on my Instagram, I received countless messages of moms freaking out. It is our nature to want to do whatever we can to protect our children, but some things truly are out of our control. I wanted to call out a few things in particular. Low socioeconomic status is an identified “protective factor” in avoiding IBD, but has many other potentially negative effects on a family. This study is viewing that data in a bubble as opposed to the whole impact of low socioeconomic status. Having more than two siblings is another “protecting factor” in IBD development. This again is something that is being looked at in a bubble. There is no recommendation to have more children for the sole purpose of protecting against IBD. The same goes for other factors such as urban living. There are some benefits in other regards when it comes to urban living. We can’t just change where we live to hopefully avoid IBD. As a mom to two little ones, there are two factors that give me a pit in my stomach. One is the risk factor of not being breastfed and the other is early life antibiotic exposure. Breastfeeding is something that is so deeply personal and challenging. Sometimes there are medical reasons (physical or mental) that prevent breastfeeding. Other times mothers are not able to breastfeed due to lack of resources or support. There are also scenarios where breastfeeding is not an option at all. This is such a complex issue and emotionally charged on both sides. As a mom, if you read this and get a pit in your stomach, try to remember that this information is again, in a bubble. Just because you didn’t breastfeed does not mean your child will have IBD. The same goes for early antibiotic usage. This is something that can be out of a parent’s control. If a baby has an infection that needs to be treated with antibiotics, that is the best course of action. There are situations where the benefit outweighs the risk and there is nothing that can change that. In conclusion, this session provided some very interesting insight and shared some low risk lifestyle changes that we can adapt to help lower our children’s risk of IBD. On the other hand, I am curious to see additional studies that evaluate these factors on the basis of risk/benefit. I also am interested to see how the findings may change if the study was conducted outside of a Western environment. What questions do you have after reviewing and reading? Are there any key points you would want to hear more about?
0 Comments
Leave a Reply. |
Blonde babe.
Millennial mom. Crohn's crusher. Mental health advocate. Sharing my raw and real journey through motherhood and navigating Crohn’s Disease. CrohnicallyBlonde is a place where I serve up my unfiltered commentary on chronic illness, mental health, pregnancy, and motherhood alongside lighter lifestyle content like beauty product reviews, travel tips, and book recommendations. My hope is that by authentically sharing my story I can help others going through similar situations not feel so alone and maybe even laugh along with me. categories
All
archives
November 2023
|
|
LET'S CONNECT ON SOCIAL
|
ContactFor press, partnerships, and general inquiries please contact: [email protected]
|



 RSS Feed
RSS Feed