|
This year for gift guides I wanted to do something a little different. Over the past year I have become a lot more cognizant about where I am spending money - less “stuff”, more quality, and supporting certain brands or businesses. Over the years through blogging/Instagram I have had the chance to learn about, work with, and share some incredible brands that I may not have gotten to know otherwise. A lot of these businesses are small businesses founded by women (often moms!), which I admit makes me love them even more. For this year’s gift guide I wanted to highlight some of these brands I’ve worked with and products I love. Everything on this list is either created/founded/run by women or in the case of the book suggestion, written by a woman. The great thing about products created by women is that they make the perfect gifts for other women in your life. They get it! So peruse my suggestions, add some ideas to both your shopping list and your own wishlist, and feel proud that you are supporting women in business this holiday season. Premium Crafted LoungewearLoungewear created by a busy mom who wanted to look put together while being comfy as heck. All of the brand’s pieces reflect that vibe. They feature cozy joggers, flattering hoodies, and comfy shorts that you can mix and match to create a perfect “mom uniform”. The material is buttery soft and the quality material elevates these pieces from typical loungewear. Some other key selling points - the cut of the sweats are more flattering than usual loungewear which keeps you from looking sloppy and the chic colors give a luxurious feel. These are my go to’s for school pick up, weekend errands, and coffee dates. The shorts have been a staple now for me to wear around the house this season. Some additional pairs are on my own wish list! Mina Baie BagsThese are high ticket, but worth the price. I have the Stevie Backpack to use as the diaper bag for the kids and it is perfect. It's durable so it stays looking structured and without wear despite being lugged around. I also love the ample pockets to organize items for quick access. It is professional enough that it can double as a work or travel bag without sacrificing style. I love the idea that a woman’s bag isn’t just for being a mom or being at work. A woman is both of these things at the same time so she should have a bag that works equally well for both. Mina Baie nails this feel with their designs and you can feel the difference. "Gutsy" by Natalie FrankeThis book is sure to inspire and a must for the women on your list. Without giving too much away, this book inspires women to not be afraid to use their unique voice, see the value their gifts bring to the world, and remain confident and resilient even when it's hard to do so. This is a perfect uplifting read to round out the year and kick off a new one.The message transcends generations so whether you are gifting for your cousin in college or your grandma, this book will speak to her soul. Port and Polish Pill BoxesThese are such a fun way to spice up an otherwise boring routine. Daily medicine doesn’t have to be so “bleh”. Not only are these a way to simplify your life, they are also so aesthetically pleasing. This is one of those things that I didn’t realize I needed and now that I have one I can’t imagine life without it. They come in a selection of chic colors and the sleek case fits well in a purse or looks great on your nightstand. Ever SkincareEverything I have tried from this brand has been phenomenal. Ever Skincare is formulated for women over 30 and designed to support skin through hormonal changes. Again, we love products by women for women. Their peel pads are a perfect stocking stuffer to add to your list or if you are looking for a larger ticket option, the At Home Facial Discovery Set is great. Oka-B FlatsIt is so difficult to find flats that are practical and stylish. If they are cute they are most likely painful and slippery, but that is not the case with Oka-b. They have a ton of styles that are trendy but don’t sacrifice comfort. They are slip resistant, easy to clean, and have support.
Hopefully these ideas gave you some inspiration and maybe even encourage you to add some items to your own wishlist. You can feel good knowing your dollars are supporting women in business and also feel confident you will be getting some great products in return. Happy gifting! xx
0 Comments
Over the summer I had the chance to get to know more about Curio Wellness and more specifically the GI by Curio™ line. I had been using the products for a while to help my GI symptoms so getting to hear more about the creation and science behind the products was enlightening. The podcast episode I did with Chief Revenue Officer, Rebecca Raphael, covered some FAQs about medical cannabis usage along with some specifics about the formulation of the GI line. You can listen to that full episode here. I also shared a post highlighting some of my favorite GI by Curio remedies. Since the podcast and post went live I have received a ton of questions as well as requests for some more in depth details on the products I love and why they work. I’ve teamed up with Curio to address some of these topics and hopefully answer the questions you all may still have! The most popular question (and the one that I immediately had when I started considering the GI by Curio line) was what makes these medical cannabis products different? How are they different from just any cannabis product you’d pick up at your dispensary? A few things to call out here… First off, the CBG in the products is a game changer. In my recent podcast episode with Dr. Morris from Duber Medical she explained how CBG is a cannabinoid that has been found to target the gut. Having a formulation with CBG, CBD, and THC is a winning combination for addressing GI symptoms. The four products found in the GI by Curio line have varying ratios of CBG, CBD, and THC concentration depending on the ideal use. Each of the products has other unique differences which I will touch on later. Another big point of difference in the GI by Curio line is the involvement of Curio’s Scientific Advisory Board in product formulation. They ensure not only product safety, but also formulation to specifically address symptoms experienced by IBD, IBS, and other chronic gastrointestinal disease sufferers. Knowing that the products are created specifically for IBD patients gave me a lot of peace of mind when trying out the products for the first time. Another question I get asked frequently is about the THC potency and impairment due to THC. These products were created truly for medical use which means they kept the levels of THC as low as possible in order to provide maximum benefit with minimal impairment. Of course, I always recommend starting with a small dose since cannabis impacts everyone differently, but the goal of these products is to provide symptom relief not impairment. This is another factor that was really important to me when choosing medical cannabis products. A lot of the medications I was prescribed to treat my GI symptoms came with other side effects, one of which was extreme fatigue. I struggled to take these medications and then continue on my daily activities. So while my symptoms may be put at bay I was unable to function normally due to the fatigue. With the GI by Curio products I am able to control my symptoms and fully function since I do not experience impairment or other side effects while using the recommended dosing of the products. The last piece I want to touch on is when to use which products. Everyone has their own routine and product combinations that work best for them. I will share mine along with some of the key benefits/why I use these products in specific scenarios. Again, this is just my personal routine, what works for you may be different, but this could be a good place to start if you are just starting out with the line. The GI Comfort Tablets are my favorite for everyday use. They have a generous dose of both CBD and CBG which provide anti-inflammatory benefits as well and antimicrobial benefits. I take these as part of my daily routine and think of them sort of as a maintenance product. They aren’t necessarily for immediate pain relief or symptom relief, but over about a week of use I started to notice an overall difference in my daily symptoms. I also noticed this helped my anxiety levels even out when I first started taking the tablets regularly. The tablets are a great starting point if you are interested in dipping your toe in the medical cannabis world. They have an extremely low level of THC so you can expect no impairment when using this product. The next product that I love is the Soothe Tincture. I recently did an Instagram post about how much I love this product. I was able to replace my prescription anti-nausea medication with the tincture, which was a huge win for me. The Soothe Tincture was formulated specifically to target nausea. I had always heard that cannabis was a great remedy for nausea, but I was never confident enough in my knowledge to choose a strain or method that I thought would work without causing any impairment. This product was the answer. All the guesswork is taken out of the process and there are specific dosing instructions so you receive maximum benefit without the impairment. This has helped me with nausea related to my IBD as well as motion sickness. You consume the droplets under your tongue and symptom relief usually starts in about 20-30 minutes. Next up is the Soothe Vape. This is a great choice for immediate relief. If I am having active pain along with nausea this is my go to. It is formulated specifically to help with both nausea and pain while also providing a calming effect. This is helpful for managing nighttime pain and getting a better night's sleep. I also find this product very effective in soothing some of my joint pain that is associated with my Crohn’s Disease. Prior to switching to medical cannabis products like this one, I was prescribed different medications from muscle relaxers to opiates. These of course are not ideal for long term use and have many side effects (as well as potential addiction risks) that come with them. I am now able to find the same if not more effective relief without the risks and side effects. As someone who was always a tablet or edible girl, the vape seemed a bit intimidating, but dispensary staff can help make sure you are good to go and comfortable with your choice. Last up are the Stimulate Chews. Not to be dramatic, but these have been life changing. They have an even balance of CBG and THC. I usually take half of a chew which leaves me feeling better without any impairment. The effects are truly incredible though. These have helped me so much with pain relief, especially when I am experiencing cramping or stomach spasms. They usually kick in about an hour after I take one, sometimes quicker if I eat a small snack with it. These are a nighttime go to for me when I am in a lot of pain. They also help to ease my anxiety (often triggered by the pain and increase of symptoms) so it is a two in one fix. These were designed to help potentially increase appetite. I was worried (like I hear from many other patients) that it will swing the pendulum in the other direction and make you outrageously hungry. For me that has not been the case at all. Instead I describe the effect as making eating more bearable. If you are a GI symptom sufferer you know how excruciating it can be to eat when you are experiencing active symptoms. This has helped me be able to eat when before it was too painful. I also find if I eat something that starts to cause discomfort, taking a half of a chew can help make digestion of that feel less painful.
I can confidently say that in my experience all four of the GI by Curio products have contributed to symptom relief and improved quality of life for me. I am able to get relief from debilitating symptoms while still being able to participate actively in life and my children’s lives. I have shared my experience with many other IBD sufferers who have also seen benefits from these products and continue to use them in their daily lives. I hope this post helps to answer questions you may have. I am always open to sharing more about my experience and answering questions about my experience as well. To round out this post I just want to say a huge thank you to Curio for being so dedicated to providing reliable products that treat symptoms that IBD sufferers experience. It has been a relief to have a trusted place to turn to for medical cannabis products I can count on. With their commitment to safety and the involvement of their Scientific Advisory Board I feel confident that I am choosing a symptom management option that works and fits my lifestyle.
Recently I had the chance to chat with the creators of FODZYME and founders of Kiwi Biosciences, Anjie and David. I met Anjie earlier this year at Digestive Disease Week where I was introduced to the digestive enzyme powder. I immediately loved how the mission of FODZYME was to make foods more accessible to those with digestive struggles. So often the recommendation is to limit foods. This can feel extremely isolating and be difficult to stick to. FODZYME’s approach is to treat the food instead of eliminating it.
In this week’s episode of the Crohnically Mom podcast Anjie and David share the science behind the revolutionary powder. We discussed what FODMAPs are (these are what FODZYME targets), how the powder works, and who it works for. We also discussed the social and mental effects intense elimination diets can have on an individual and the benefit of having another option to try.
I have been using the powder when I eat certain foods since I discovered the product earlier this year. I know it personally works for me, but I loved being able to get an insight into why it works. I also really enjoyed hearing from Anjie and David about their journeys that led them to found their company and create FODZYME. Their passion for the product is inspiring and I am so grateful for their work.
You can listen to the full conversation in this week’s episode of Crohnically Mom. It is available on Spotify, Apple Podcasts, and Soundcloud. Additionally, if you are interested in trying FODZYME, they have provided Crohnically Blonde readers and Crohnically Mom listeners with a discount code (CROHNICALLYBLONDE) for 20% off your order! I have never had thick luscious hair, but have been able to rely on styling products and hair extensions to give me the look I want with no issues. After having my daughter, though, my postpartum hair loss felt more extreme and I panicked especially about the hair loss, especially close to my hairline. Hair extensions work well for length and volume, but once thinning and loss hit the hairline, it's time to consider some additional options. This is a big area of insecurity for me so I was on a mission to find some products that could help me out. *Vegamour enters the chat* I had seen posts raving about the products on social media, but wanted to do some more research myself. I was delighted to find that they are vegan, cruelty free, and don’t have all of the baddie ingredients we all hear about (sulfates, parabens, etc.). I am careful not only about what I use on my real hair, but my extensions as well (they’re expensive so I do not play around!). Luckily it seemed like these products were a good solution for both my natural hair and my faux locks. For the past month I’ve been using The Everyday Kit, which includes GRO Revitalizing Shampoo, Conditioner, and Dry Shampoo. I’ve been very impressed with the results already. Here are my highlights:
These are now a staple in my haircare routine and I would recommend them to any postpartum mom who is going through the same thing. I am not still breastfeeding, but based on the ingredients these are products I would be comfortable using while breastfeeding and even while pregnant. Of course, talk to your doctor and make your own decision, but for me these get the stamp of approval. I also want to mention, over the years I’ve had chats with many other women who have experienced thinning hair or hair loss during a time when their IBD was really bad. I went through this for years and know how much of a blow it can be to your confidence. If you fall in that bucket, this could be a haircare line for you to look into. Especially with the assurance of clean ingredients you can confidently use the products without worrying about scalp irritation or exacerbating any other skin condition (also common with IBD/autoimmune diseases). When it comes to price point, the products are on par with other high end hair care brands. I feel good about making the investment in these, because I know exactly what I am getting thanks to the transparency around ingredients and IT ACTUALLY WORKS. Worth. Every. Penny. They also offer mini sizes (which you know I love) of the shampoo, conditioner, and dry shampoo. So if you want to try before grabbing the full size versions, that is an option. You can take a deep dive into the science behind the products and their ingredients, here, and shop the full product line on their website. Next up on my list to try is the GRO Hair Serum… xx Antibiotic exposure is a risk factor that came up repeatedly during my time at Digestive Disease Week. I mentioned it in my recap of Pediatric IBD sessions, but there were many other sessions where it was a focus as well.
I surveyed my followers with IBD and about ⅓ of them said they think their onset of early IBD symptoms correlated with a time of heavy antibiotic usage. Of course, this isn’t a scientific study, but I thought it was interesting that this is a factor the IBD community can identify firsthand. The CDC has identified the overprescribing and improper use of antibiotics to be an issue in the United States. In a 2022 study, the CDC reported that at least 28% of all antibiotics prescribed in an outpatient setting were unnecessary. That is 28% of people unnecessarily exposed to a key IBD risk factor. A lot of our country’s reliance on antibiotics as a first line of treatment can be linked back to the flaws within our healthcare system. Instead of focusing on an underlying issue, our culture is prone to immediately jumping on a “quick fix.” Providers are incentivized to see as many patients as possible. It is easier and quicker to write a prescription and send a patient on their way as opposed to taking a holistic look at the patient’s health to identify other potential causes for their symptoms. This isn’t to fault providers. There are many of them who wish to take a more holistic approach, but the way our healthcare system works doesn’t allow them to. Patients are not blameless in this either. As patients we are conditioned to have a medicine to fix just about everything. If we go to a doctor for a cold and they tell us to go home and get some rest, we leave grumbling about how we made the trip and made a copay just to be told to go home and get some rest. It is almost like we want them to unnecessarily tell us we have a sinus infection so we can get some antibiotics and feel like we are doing something to heal quicker. I have actually heard people leave urgent care complaining that they couldn’t get an antibiotic prescription and planning to just “go see another doctor until they get one.” Moving away from antibiotic overuse is a cultural shift. It can’t just be on the provider or patient side, it has to be a collaborative effort. There also needs to be more openness in the discussion of natural (or non prescription remedies). So often if you mention a natural or holistic treatment, a provider will dismiss the suggestion. Of course sometimes these treatments are totally bogus and not worth your time, but in other scenarios they could have potential benefits with few to no downsides. For many of these holistic treatments, we are still lacking evidence based research that support them. It is responsible of a provider not to suggest something without supporting evidence, but it is also irresponsible for them to shut down the conversation altogether. With the CDC pushing us toward less antibiotic use, will there in turn be more money and research dedicated to other holistic treatments? The last factor I want to touch on is insurance coverage for medications. So often, antibiotics are not only a seemingly “quick fix,” but also a cheap one. Insurance companies are more likely to cover antibiotics than they are any type of alternative treatment. Even if a doctor recommends something like acupuncture to help with sinus pain, it is not likely to be covered under many insurance plans. Do you know what is covered? That 7 day supply of an antibiotic to treat a “potential sinus infection.” Again, I want to reiterate that this is not the fault of providers or the fault of patients. We as a society have gotten to this point and need to recalibrate on what is best for our country’s health as a whole. I am also a firm believer that antibiotics are 100% necessary in some situations. I will give my kids antibiotics if they need them. I take antibiotics when I need them. Antibiotics can save lives when used appropriately. Just like so many things in American culture, we have taken them to one extreme. If we can find a way to balance antibiotic use, I predict our society will see positive health benefits. To get there though, we have some big changes that need to be made. xx Yesterday my podcast episode with Rebecca Raphael from Curio Wellness dropped. We chatted about using cannabis to help with GI symptoms (you can listen to it here). When I first got my medical marijuana card and walked into a dispensary I had absolutely no clue what to look for or what to ask. Over time I had conversations with my doctors and professionals who are knowledgeable about medical marijuana and got a lot more comfortable with the topic.
I wanted to pass along some tips for those of you who may be interested in utilizing medical cannabis. As always, please remember that I am not a medical professional so please do not take this as medical advice. Always consult with your provider before starting a new supplement or treatment. This disclaimer leads right into my first tip. 1. Talk to your doctor. From my conversations with various GI providers about medical marijuana, the biggest take away is talk to them about it! They are not judging you and they genuinely want to know for important reasons. Just like any other herbal supplement it’s important to share with your provider so they can check for any potential interactions and track your symptoms. Also, providers can get a better idea of the impact of the other medications you are taking. For example, if an IBD patient is using medical cannabis and seeing symptom improvement, but not telling their provider this could cause confusion. The provider may attribute symptom improvement to another treatment they are on as opposed to the medical cannabis. It is important for providers to have a full picture of what you are doing to treat your symptoms so they can best advise and treat you. Just some of my own words of advice here: if you feel judged or shamed by your provider, it may be time to find a new one! 2. Find a reputable dispensary and ask them questions. That’s what they’re there for! Dispensary staff are incredibly knowledgeable and many have a genuine passion for teaching others about cannabis. They are there to advise you on which products will meet your needs and can walk you through many different options. Especially when you are first starting out it can be hard to decipher the difference between strains, cannabinoids, terpenes, etc. (Rebecca Raphael from Curio Wellness does a great job breaking that down on this episode of the podcast.) They can make sure you get the best product for what you are looking for and the best consumption method for your situation. 3. Start slow - ease into it If you are just starting out, don’t overdo it. There are many low dose cannabis products that can give you the desired effects without any impairment. The issue new users run into sometimes is forgetting that it can take a bit for the effects to kick in. If you are ingesting cannabis products or using them sublingually, they can take even up to two hours to really start working. If a patient is not aware of this, they may think their original dose is not working and consume more. This could cause them to feel unwanted effects like impairment. Cannabis dosing is different for everyone so start small and see what works for you. Just because your friend takes one amount doesn’t mean you will need the same dose. 4. Don’t be afraid to try different products There are many different products on the market and an ever increasing number of new ones to try. Don’t be afraid to try a new product to see if it works for you. Your dispensary can help guide you as to which products are similar to ones you already use or which ones you may like. You may discover new product lines or symptom specific products that you didn’t know about before. Some, not all, dispensaries have refund or exchange policies to help offset the financial risk of trying a new product. Ask about this to see what your dispensary offers. 5. Keep an eye out for new research As cannabis grows in popularity and becomes legal in more areas the research will continue to increase. There are many professionals dedicated to providing evidence based research on cannabis and are working hard to do so. Keeping up with the latest in cannabis news and research can alert you to new findings that may impact your use. xx Medical cannabis is a topic I’ve wanted to talk about for a while now, but never actually did because I was scared of the backlash. You’d think that someone who talks about their bowel movements on a public platform, sharing my experience with medical marijuana wouldn’t cause any pause, but that wasn’t the case. Judgment around this topic can be brutal, especially in the mom community. As in most situations, judgment stems from fear and lack of education. I believe that if people were properly educated on the benefits and usage of medical cannabis the narrative would change. I think we are seeing the tides turning in that direction, and I hope to be a part of that. That is why I finally decided to start sharing my personal experience with medical marijuana. Seeing as education is paramount, I wanted to make sure I kicked off my discussion of this topic with someone who is an expert. On this week’s episode of Crohnically Mom, I sat down with Rebecca Raphael, the Chief Revenue Officer at Curio Wellness to discuss all things cannabis. Curio Wellness is a Maryland based cannabis company devoted to providing safe, effective cannabis products. She gave a crash course in what you need to know if you are looking to give medical marijuana a try, we chatted about products that are best for GI conditions, and she debunked some common misconceptions about cannabis. She shared so many useful pieces of information that are great to know whether you choose to incorporate medical marijuana into your treatment program or not. We also got into topics like how to address judgment over your choice to use medical cannabis as well as how to talk to your kids about cannabis as it becomes more widely accepted. The conversation was incredibly valuable. As a mom Rebecca just GETS IT. Hearing the story of her and her family’s involvement with Curio was also so interesting to hear. I specifically reached out to Curio Wellness to chat about this topic because they are the products I, personally, use the most. They have a whole line dedicated to GI symptoms, which we get into a lot of detail about on the podcast. These have been a game changer for me as I have navigated more severe Crohn’s symptoms over the past couple of months. What I currently use from Curio Wellness are:
GI Comfort Tablets
The scoop: Each tablet has a minimal amount of THC so you can get the benefits without the impairment. These are meant to be taken twice daily for the management of GI symptoms related to GI disorders. These won’t do the trick if you are looking for immediate relief, but do help if you are consistent with taking them everyday! These I like to think of as the long game!
GI Stimulate Chews
The scoop: Each chew contains 20mg CBG and 5mg THC. These are designed to have a relaxing effect on the GI system. These are a game changer for GI pain. They help to calm stomach spasms, lessen gas pain, and ease my joint pain. They also make eating just more comfortable in general. For me the 5mg of THC can make me a bit sleepy so if I need one of these during the day I will usually just take half of a chew.
GI Soothe Tincture
The scoop: This is oil that you place under your tongue. Each dose has 5mg of THC as well as 5mg CBD and 5mg CBG. I personally love this to take instead of an anti nausea medication or to help calm stomach spasms. It was formulated specifically to help with nausea and it definitely does what it is supposed to do. For more information on Curio Wellness you can visit their website, here. You can listen to my chat with Rebecca on Crohnically Mom, here.
Recently I had the chance to sit down with Tamara Duker Freuman, registered dietician and GI nutrition expert. I interviewed her for my podcast, Crohnically Mom, and she provided helpful insight into navigating nutrition and IBD. You can listen to the interview here.
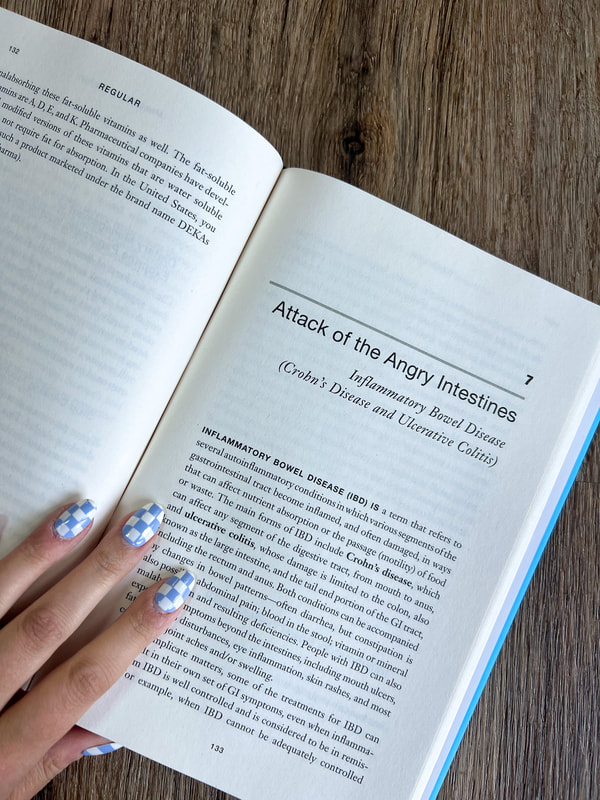
How I was introduced to Tamara was through her newest book “REGULAR”. It is one of the most helpful books about GI symptoms I have ever encountered. Many books focused on addressing GI symptoms focus on things you are doing wrong – the wrong diet, not getting enough sleep, eating “bad” foods, etc. This is demeaning for a reader, especially one with IBD. A lot of the time we have tried everything and it hasn’t worked so the generalized assumption that people with GI issues can “do something about it” is incredibly frustrating. “REGULAR” has a totally different tone that I would describe as empowering.
Tamara starts the book by providing a thorough, yet completely understandable, explanation of how your digestive system works. This is one of my favorite parts of the book and we were only in the first few pages. She breaks down the anatomy in a way that doctors rarely do during a 15 minute appointment or if they do, it usually isn’t communicated in a way that is, excuse my pun, digestible. This knowledge is so crucial because it allows someone experiencing GI symptoms to accurately explain to their doctor what they are experiencing. It also saves them from hours of Google research and perusing through unverified information. This is straight to the point, reliable information about what the heck is going on in your digestive tract. After the helpful introduction, Tamara guides you through a quiz. The quiz allows you to answer questions about your symptoms and narrow down the chapters that could be most relevant to you. Most people are reading this book not for their interest in GI disorders, like me. They are looking for help, a solution. This quiz helps them get to the most relevant information quickly and because of that, I love this style of book for non-fiction reads. The chapters address a range of GI symptoms/issues from Irritable Bowel Syndrome, to pelvic floor dysfunction, to Inflammatory Bowel Disease. The IBD section was where I spent most of my time. I was looking forward to hearing Tamara’s recommendations, but I admit at first I was a bit nervous. Usually I get nervous reading any book that mentions “diet”. So often they are filled with unrealistic overhauls of your current lifestyle that put foods into categories of “good” and “bad”. As someone who has struggled with an eating disorder in the past, this can be very triggering and also just not helpful. “REGULAR” is refreshing as it doesn’t do either of these things. Tamara explains how foods navigate through your system and how they are absorbed. She never says “do not eat this.” Instead she suggests ways to make certain foods more tolerable (e.g. changing their consistency). You will hear in our conversation, how passionate in her practice Tamara is about providing customized nutrition counseling. She isn’t about just throwing a blanket “fix all” meal plan out there and hoping it works, so she doesn’t do that in “REGULAR” either. Overall, this book is full of fresh takeaways even for someone who is not new to being a GI patient. Tamara’s approach is meant to leave the reader feeling empowered, whether it’s speaking to their provider, looking for answers to their symptoms, or exploring a type of food they always thought was out of reach. This will now be a “go to” recommendation from me for anyone suffering from a GI condition. You can hear my in depth conversation with Tamara on this week’s episode of Crohnically Mom. You can also grab Tamara’s book, “REGULAR”, on Amazon. xx Traveling is one of my greatest joys in life so when I was diagnosed with Crohn’s Disease, I refused to let my symptoms prevent me from doing what I love. Flying can be a big source of anxiety for those with Inflammatory Bowel Disease. There are many factors that can play into the feeling, but one of the most common ones is the concern about not being near a bathroom. Flying is also a necessity in some situations - work travel, family visits, etc. Your travel schedule and GI symptoms unfortunately don’t coordinate to make sure you have a comfortable experience. That being said, anything to reduce the anxiety around flying when experiencing GI symptoms is a welcome suggestion. One of the most simple ways to combat a common concern is to make sure you are positioned near a bathroom on the flight. On certain airlines, you can choose your seat ahead of time. This means locking in that prime aisle seat right next to the facilities. No stepping over other passengers mid bathroom emergency and you are close by so you won’t have to fumble down the aisle as you’re trying to make it to the facilities. This is great for airlines that offer this preselection option.This isn’t always the case, though. I most frequently fly Southwest which has open seating (i.e. no preselected seats). This has caused me a lot of anxiety over the years - panicking when I didn’t get an early boarding group, having to ask passengers to switch seats with me and awkwardly explaining why, and trying to do anything I could to avoid having to use the bathroom on flights (which was not very effective). A few years ago, I saw some fellow IBD patients share a travel tip and it instantly changed traveling for me. Southwest offers disability preboarding and Inflammatory Bowel Disease is a disability. When I first found this out, I was in the stage of denying IBD was a disability that impacted functions of my life, but now looking back I wish I would have accepted this sooner so that I could utilize the resources that are there for IBD patients. That is why they are there, to help us! I check in like I normally would for my Southwest flight and once I get to the gate, I speak with the gate attendant. I explain that I require disability boarding due to my Crohn’s Disease and need to be seated next to a bathroom. I always have my doctor’s note on hand to show if it is needed. The gate attendant updates my boarding pass to list preboarding status and I am good to go.
Disability preboarding includes passengers with all types of disabilities. This means you will often be boarding with wheelchair users and other passengers with mobility challenges. I understand that for them it is more necessary that they have the seats closer to the front of the plane, while for me I have the option of sitting near the rear bathrooms. That being said, I make sure not to take the front seats if they are needed by others. When I board the plane, I confirm with a flight attendant that there are functioning bathrooms at the back of the plane and head on back to secure my seat. This small tweak to my travel routine has made a significant impact on my anxiety level while traveling. The knowledge that I will be able to have easy access to a bathroom while in the air is a huge comfort. I recently realized how many fellow IBD patients don’t know that this is an option. I didn’t for the longest time, until I saw a patient advocate share the information ( I wish I remembered specifically who because I would definitely shout them out!). I know how much that information helped me so I want to help spread the word that Southwest does offer this option to support passengers with visible AND invisible disabilities. As I mentioned before, I went through a period where I was in denial that IBD was a disability. For a while when I started to actually utilize these types of programs, I would feel embarrassed. I thought people were looking at me strangely because they couldn’t see that I was sick. I went out of my way to awkwardly over justify why I needed certain accommodations. It has taken me years to work through and I still struggle with it, but I have gotten a lot more comfortable. Just because my condition isn’t visible doesn’t make me any less deserving of the programs that are in place to assist people like me. I am not saying to utilize every offered accommodation “just because,” but if it is something that will impact your condition, symptoms, or quality of life, you should feel empowered to use these resources that are there for you. As an IBD patient did you know that this was an option for you? How would an accommodation like this impact your travel experience with IBD? xx
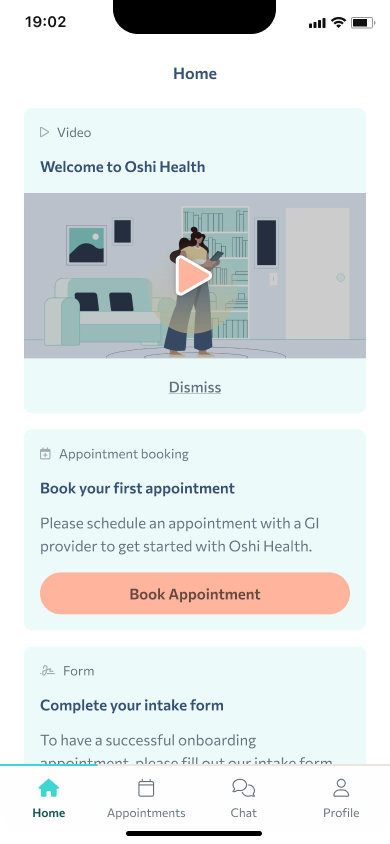
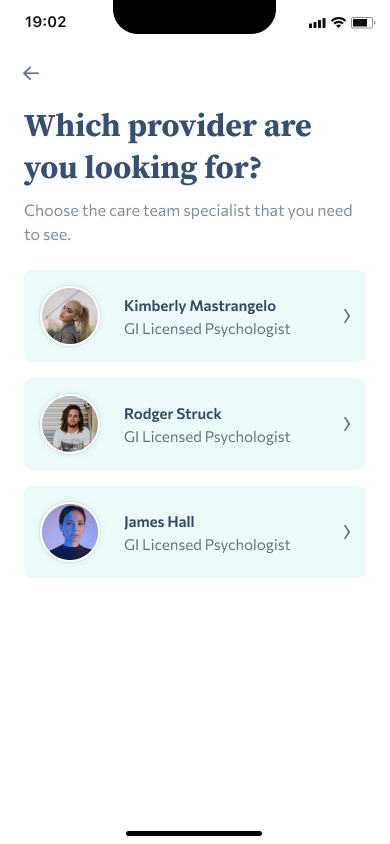
At the beginning of my IBD journey, I had the pleasure of working with Oshi Health in their early days. At the time, they were mainly a tracking app for GI symptoms. My mom and I attended a user research group in New York and met with some of the consulting physicians. This was the first time I was introduced to the concept of integrative care. It wasn’t something that was a reality yet for many patients, but the idea that providers could work together and treat the whole person was a positive one.
Almost 5 years later, I had the pleasure of sitting down with Michael Currier, a GI Physician Associate at Oshi Health, to get an update on how the company and the app have evolved. Oshi Health has grown from a tracking app for GI conditions to a full service option for receiving integrative GI care. Through the app, you are matched with an Oshi GI provider who you see virtually. The appointments are on average around 45-minutes as opposed to the usual in office 10-15 minutes that are standard practice for most of us. Your provider gets to really know you and dig into the whole story your body and symptoms are telling. They can order labs or diagnostic procedures for you with their local partners (they have a scheduling team that takes care of this for you!), and you are matched with an entire team of providers at Oshi. They understand that the best GI care is multifaceted and consideration needs to be given to the effects both diet and mental health have on GI conditions. Through Oshi, you are paired with a Registered Dietician and a GI Psychologist to help you feel better from all angles. The best part, in my opinion, is that your GI provider, dietician, and psychologist all work together behind the scenes to collaborate on the best care plan for you.
A few other highlights for me are: they will work with a doctor you are already seeing if you want additional support, but aren’t ready to make a complete switch and you have access to your Oshi team via chat so you never are without a line of support. Another important call out is that they partner with many insurance companies that will cover your care through Oshi.
On an individual level, Oshi Health is changing the game for patients. They are breaking down barriers of accessibility when it comes to GI care. They are empowering patients by treating them as a whole person, not just patients. This is also revolutionary for our healthcare system in general. It is rare that there is so much collaboration between different providers despite how much of a positive impact it could make. Oshi Health has designed a model that flips that statement on its head and is challenging what we currently accept as the status quo. You can listen to my conversation with Michael Currier from Oshi Health on this week’s episode of Crohnically Mom. He explains more about the benefits of integrative care, how Oshi is creating more accessible GI care, and how their model gets patients better. |
Blonde babe.
Millennial mom. Crohn's crusher. Mental health advocate. Sharing my raw and real journey through motherhood and navigating Crohn’s Disease. CrohnicallyBlonde is a place where I serve up my unfiltered commentary on chronic illness, mental health, pregnancy, and motherhood alongside lighter lifestyle content like beauty product reviews, travel tips, and book recommendations. My hope is that by authentically sharing my story I can help others going through similar situations not feel so alone and maybe even laugh along with me. categories
All
archives
November 2023
|
|
LET'S CONNECT ON SOCIAL
|
ContactFor press, partnerships, and general inquiries please contact: [email protected]
|




























 RSS Feed
RSS Feed